Sleep apnea, a prevalent sleep disorder affecting a significant portion of the adult population in the United States, disrupts sleep and overall health. It’s estimated that sleep apnea impacts between 10% and 30% of adults. Positive Airway Pressure (PAP) therapy is a cornerstone treatment, encompassing Continuous Positive Airway Pressure (CPAP), Bi-level Positive Airway Pressure (BiPAP), and the more advanced Adaptive Servo-Ventilation (ASV).
PAP machines function by delivering pressurized air through a mask, keeping airways open during sleep. This consistent airflow helps stabilize breathing, reduces daytime sleepiness, and significantly enhances the quality of life for individuals managing sleep apnea. CPAP devices, the most basic PAP form, provide a constant air pressure during both inhalation and exhalation. BiPAP machines offer two pressure settings, one for inhaling and another for exhaling. While effective for obstructive sleep apnea, Adaptive Servo-Ventilation (ASV) machines are particularly beneficial for those also experiencing central sleep apnea.
Understanding Adaptive Servo-Ventilation (ASV) Machines
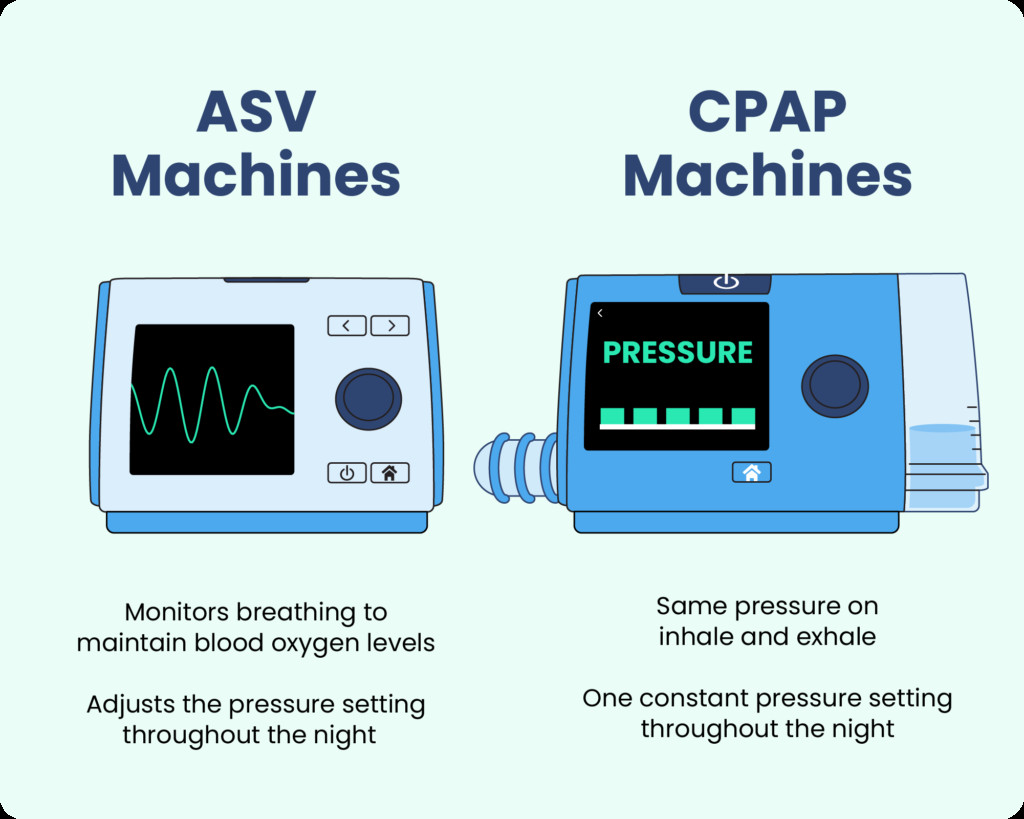
Adaptive servo-ventilation (ASV) machines are sophisticated devices designed to monitor and stabilize breathing throughout the night. These machines deliver personalized air pressure that dynamically adjusts to an individual’s unique breathing patterns. Unlike CPAP machines that provide a constant level of air pressure, ASV therapy adapts in real-time, making it particularly effective for complex breathing disorders.
The key distinction lies in the dynamic air pressure delivery of ASV machines. While CPAP maintains a steady pressure, ASV machines continuously analyze breathing patterns and modify air pressure accordingly. This adaptive approach ensures that the airway remains open and breathing is regularized, addressing both obstructive and central sleep apnea events.
Both central and obstructive sleep apnea are characterized by pauses in breathing, known as apneic events. Obstructive sleep apnea occurs when the airway becomes physically blocked or narrowed, often due to relaxation of throat muscles. Central sleep apnea, however, arises from the brain’s failure to send proper signals to the respiratory muscles, hindering breathing effort. Complex sleep apnea, also termed treatment-emergent central sleep apnea, can develop in some individuals with obstructive sleep apnea while using CPAP therapy.
Researchers suggest that CPAP therapy might inadvertently trigger central apneic events in susceptible individuals. For those with highly sensitive respiratory systems, CPAP-induced reductions in blood carbon dioxide levels or lung expansion could signal the brain to reduce breathing effort unnecessarily. This issue can be exacerbated in individuals with congestive heart failure, where the heart’s response to CPAP therapy may further complicate breathing regulation.
While some individuals adapt to CPAP therapy and these central apneic events resolve, ASV machines offer a solution for persistent cases. By automatically decreasing air pressure when normal breathing is detected, ASV devices prevent the brain from suppressing breathing due to perceived low carbon dioxide levels. Furthermore, ASV machines maintain a baseline air pressure and can increase pressure as needed, effectively managing obstructive sleep apnea events as well.
How Adaptive Servo-Ventilation Machines Work
Like CPAP machines, ASV systems consist of a face mask, a machine unit, and a connecting hose. The mask, worn during sleep, can cover the nose and mouth or just the nose, depending on individual needs and preferences.
The ASV machine’s core function is to continuously monitor breathing throughout the night. Using advanced algorithms, it detects when breathing slows or becomes shallow. In response, the machine promptly increases air pressure to restore normal breathing patterns. Once normal breathing is re-established, the ASV machine reduces the pressure, often maintaining a minimal baseline support level to facilitate consistent breathing.
This responsive mechanism makes ASV therapy particularly beneficial for individuals who experience discomfort or do not respond adequately to CPAP therapy. The variable air pressure delivery of ASV can alleviate the discomfort some users experience with the constant pressure of CPAP, potentially improving treatment adherence and overall effectiveness.
 person stretching
person stretching
This image depicts a person stretching, which is relevant as comfortable breathing during sleep, facilitated by devices like ASV machines, contributes to overall well-being and physical comfort.
ASV Therapy vs. CPAP Therapy: Key Differences
In contrast to ASV machines, both CPAP and standard BiPAP devices deliver air pressure in a pre-set manner. CPAP provides a constant pressure, while BiPAP offers two fixed pressure levels for inhalation and exhalation.
The adaptive nature of ASV machines sets them apart. They utilize sophisticated algorithms to learn and respond to an individual’s breathing patterns throughout the night, dynamically adjusting air pressure as needed. This personalized approach is the fundamental difference between ASV and other PAP therapies.
 An example of an ASV machine next to a CPAP machine.
An example of an ASV machine next to a CPAP machine.
This image visually contrasts an ASV machine and a CPAP machine, highlighting the different technologies and potentially different user interfaces associated with each type of sleep apnea therapy device.
Both ASV and BiPAP machines can provide a backup respiratory rate, which is crucial for supporting breathing during central apneic events. However, ASV machines excel in this aspect as their backup rate can be personalized and adjusted based on continuous feedback from the individual’s breathing, offering a more tailored and responsive support system.
Potential Risks and Side Effects of ASV Therapy
While ASV therapy is a valuable tool, it’s not universally recommended. A significant contraindication is for individuals with a specific type of congestive heart failure characterized by reduced ejection fraction, which impacts the heart’s pumping efficiency. Experts advise against using ASV to treat central sleep apnea in these patients due to potential risks.
Similar to CPAP machines, ASV machines can cause certain side effects and discomfort, including:
- Aerophagia (air swallowing)
- Nasal Congestion
- Sleep disruption due to mask discomfort
- Dry mouth
- Eye irritation
- Mask leak
- Mouth leak
- Nostril irritation
- Skin irritation or pressure marks from the mask
Using a humidifier with the ASV machine can help mitigate symptoms like dry mouth and nasal congestion, enhancing comfort and therapy adherence.
Compared to CPAP therapy, ASV machines are generally reported to be less likely to induce feelings of claustrophobia when exhaling against pressurized air. This sensation is a common reason for CPAP therapy discontinuation, making ASV a potentially more tolerable option for some individuals.
It’s important to note that research on the long-term risks and side effects of ASV machines is still relatively limited. Furthermore, the proprietary algorithms used by different manufacturers to determine airflow rates can vary, making direct comparisons between ASV models challenging.
Who Benefits Most from Adaptive Servo-Ventilation?
ASV therapy was initially developed to address Cheyne-Stokes respiration, a breathing pattern associated with heart failure, characterized by cycles of hyperventilation followed by periods of breath-holding. Beyond this, ASV therapy is used to treat sleep-disordered breathing in individuals with various conditions, including:
- Central sleep apnea (CSA), including CSA stemming from stroke, kidney failure, neurological disorders, or opioid use.
- Complex sleep apnea, or treatment-emergent central sleep apnea, that emerges during obstructive sleep apnea (OSA) treatment.
- Mixed sleep apnea, which involves a combination of obstructive and central apneic events.
BiPAP and ASV therapies have demonstrated greater effectiveness than CPAP therapy in managing drug-induced sleep-disordered breathing, particularly relevant for individuals using opioids for pain management or with a history of drug abuse. There is also growing interest in utilizing ASV therapy to improve breathing in individuals with central sleep apnea resulting from neurological disorders. Additionally, ASV therapy can be a beneficial alternative for individuals who do not respond adequately to CPAP treatment, such as those who experience both chronic complex insomnia and obstructive sleep apnea.
Typically, CPAP therapy is considered the first-line treatment for sleep apnea due to its proven efficacy for obstructive sleep apnea and lower cost compared to ASV therapy. However, ASV therapy becomes a valuable option when CPAP is ineffective or not well-tolerated. Many individuals find ASV machines more comfortable, which can enhance long-term adherence to therapy.
Regardless of the type of PAP device used, consulting with a healthcare provider is crucial for addressing any discomfort or issues experienced during sleep apnea treatment. Doctors can adjust machine settings or recommend alternative devices to optimize breathing and sleep quality throughout the night, ensuring the most effective and comfortable therapy experience.